Learning Outcomes
After this course, participants will be able to:
- Identify single sided deafness and list challenges faced by patients with single-sided deafness (SSD).
- Identify 3 advantages of a bone conduction system relative to other treatment options.
- Describe the treatment pathway with Baha 5 technology for their SSD patients.
Introduction
SSD Defined
Common Causes of SSD
The possible etiologies of SSD are varied, and may be the result of congenital issues, diseases or trauma. It could also result from a previous medical intervention, such as acoustic neuroma or cholesteatoma. It may be determined that the cause of SSD is idiopathic. Regardless of the cause, individuals with SSD struggle with perception of speech and environmental sounds. Additionally, patients with SSD can struggle with social situations and often report retreating from small and large group conversations. This presentation is focused on single sided deafness in adults, but SSD can happen at any age. The first step is taking action and not letting the patient’s hearing loss go untreated.
Impact of SSD
Now that we have a common understanding of SSD, let’s discuss the impact of hearing with only one ear. As Audiologists, our common goal and the desired state for our patients is for them to hear bilaterally, with two ears. It’s important for us to not only talk about how unique the SSD patient may be, but also the impact of that type of hearing loss on the patient's daily life.
Binaural hearing functions may provide important listening features, such as sound localization, lateralization and the ability to separate and select verbal messages from the background signal and summation effects (redundancy of auditory input). Due to the profound sensorineural hearing loss in one ear, SSD patients experience monaural hearing, or only hearing with one ear. Listening with only one ear requires increased effort, which can be tiring and detrimental to learning.
Speech perception in noise challenges all individuals with hearing loss of any degree or type, but perhaps even more so for individuals with single-sided deafness. They often find it hard to understand speech and sounds, especially in noisy environments. Furthermore, they experience difficulty in determining the direction of a sound's location. Many SSD patients may also suffer from tinnitus, headaches and balance problems.
Hearing loss can have an impact on an individual's safety, as well as in social situations. According to McLeod, Upfold and Taylor (2008) patients who contracted single-sided deafness following vestibular schwannoma surgery reported that a limited ability to discern sounds led to social isolation. Furthermore, with regard to the safety aspect, in a survey of nearly one thousand SSD patients who were asked to report how their symptoms affected their lives, around half of those polled said that they experienced difficulties as a pedestrian due to SSD (Figure 1). Interestingly, they also reported that they could not interact as part of a group, and felt socially excluded. Another 41% reported severe difficulty using the phone, and 39% said that SSD had made work more difficult for them.
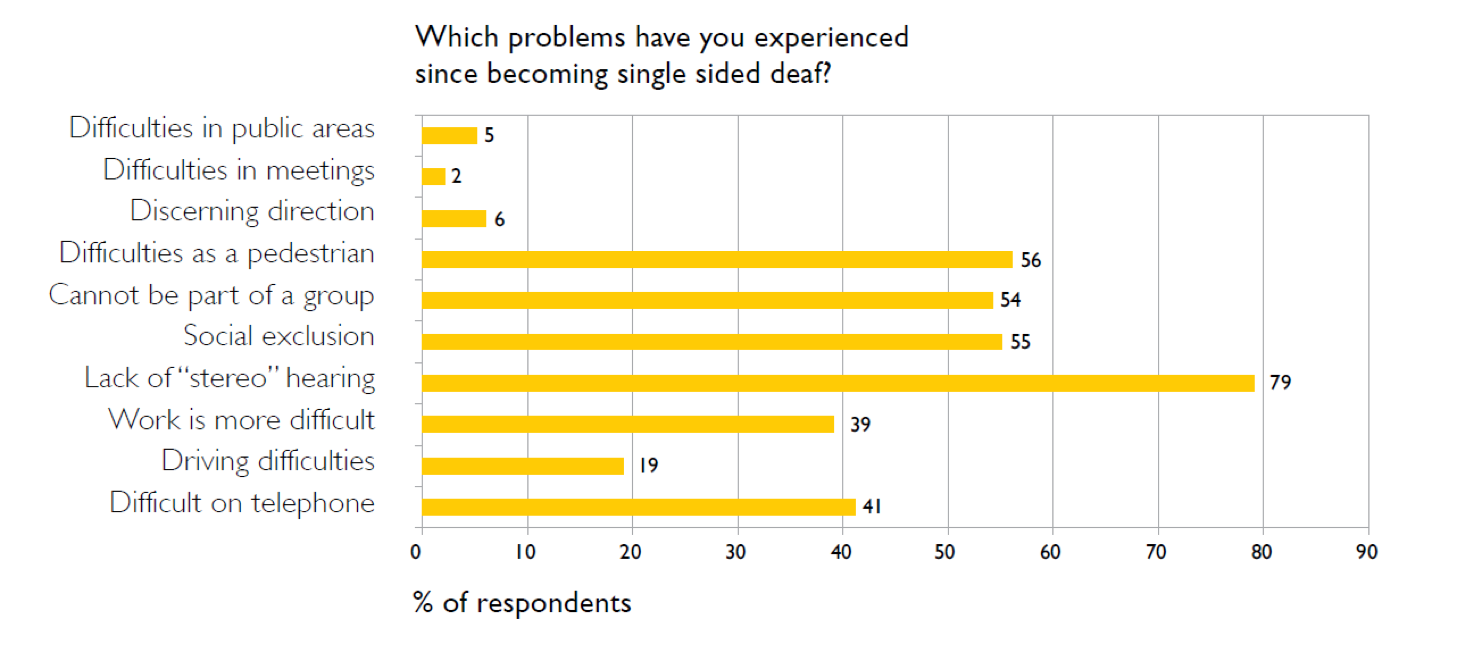
Figure 1. Safety and social impact of SSD. Data from survey contained in "Hear the other side: A report on single-sided deafness." Available from Cochlear, article E80414A.
Figure 2, illustrates SSD, in this case a damaged cochlea on the left and a normal cochlea on the right. This image illustrates the ways in which the high and low frequency signals are impacted when delivered on the individual’s left (or poorer) side. High frequency sounds are often lost in a person with SSD due to the head shadow effect.
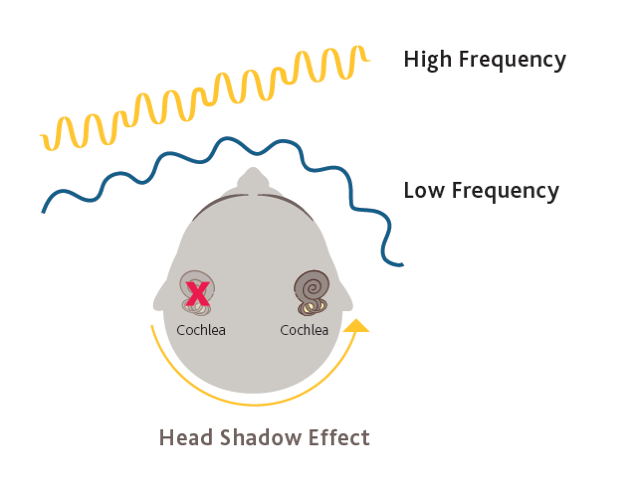
Figure 2. Head shadow effect.
Treatment Options for SSD
- Patient remains untreated
- CROS hearing aids (contralateral routing of signal)
- Steroids
- Medical intervention (surgery, as in acoustic neuroma, or blockage of the ear)
- Bone conduction devices - Baha System
- What are the patient's motivations and expectations?
- What is the cost to the patient?
- What are their cosmetic needs?
- What level of power is needed?
- Do they want a simple solution?
Comparing Treatment Options for SSD
Cochlear Baha System
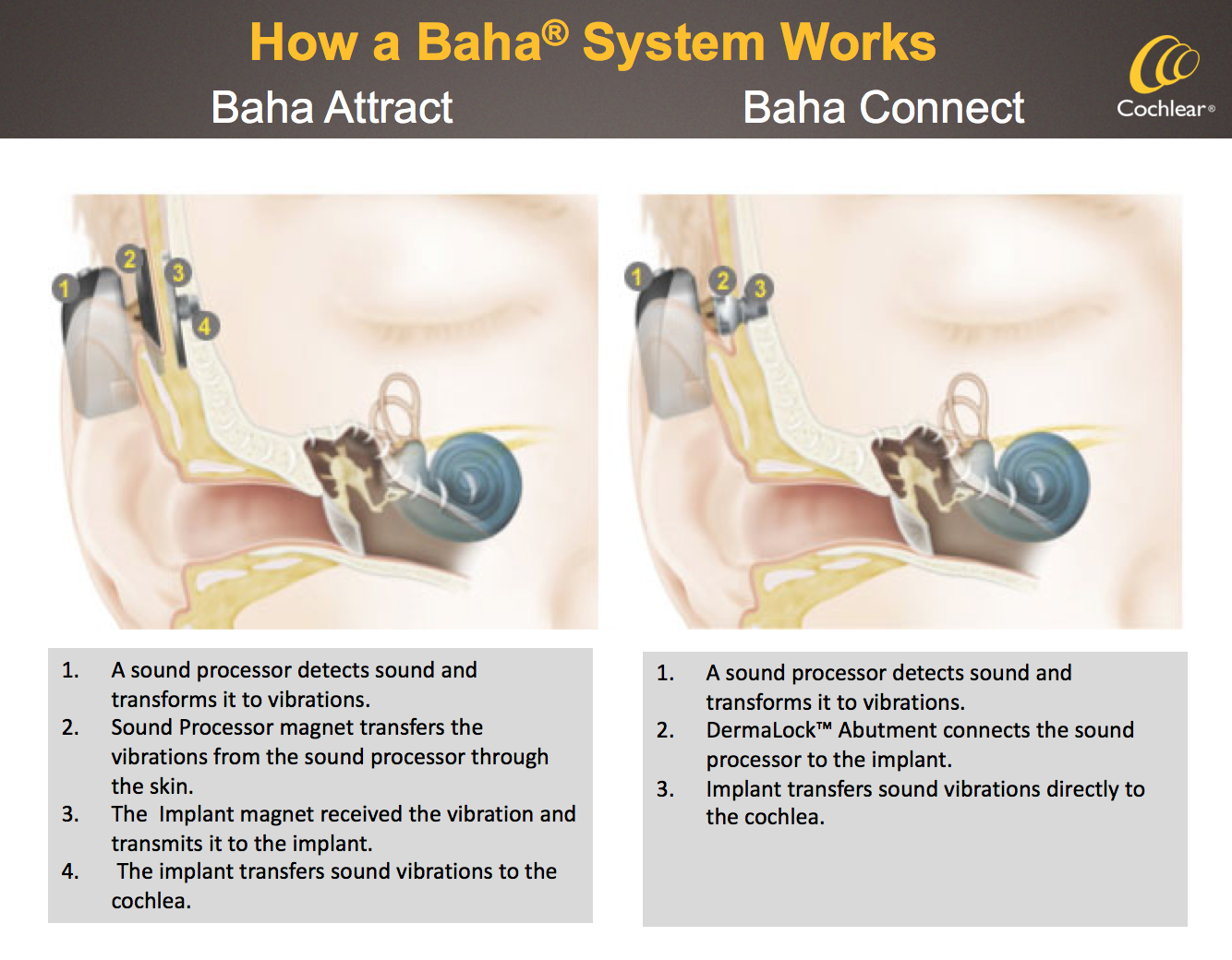
How it Works
Clinically Proven Patient Benefits
- Improved speech understanding in noisy environments. Studies have found that patients wearing Baha implants have experienced statistically significant improvements in audibility and speech understanding in noise and in quiet.
- Helps to lift the head shadow effect.
- Reduces the psychosocial consequences associated with hearing impairment.
- Long-term patient satisfaction and hearing benefits.
Baha System vs. CROS Hearing Aids
- There is no hardware in or occlusion of the hearing ear.
- There is no need to wear hearing devices on both ears.
- Patients can hear better in noise.
- The Baha System offers improved sound quality due to direct bone conduction.
- It is more useful in a variety of listening environments experienced in daily life.
Other Important Patient Benefits
Baha System Evaluation for SSD
So far, the topics we have covered include a review of SSD, an overview of the impact it may have on an individual treatment options, and how our clinically-proven Baha System can be a great choice for patients with only one functioning cochlea. Let’s now discuss how you might identify patients in your clinic, as well as how your referring partners might help to find these patients and send them on to your clinic for comprehensive care.
- Step 1: Candidate Criteria
- Step 2: Audiometric Testing
- Step 3: Benefit Evaluation
- Hearing-in-noise testing
- Softband demonstration
- Subjective assessment
- Step 4: Counsel the Candidate
- Fitting considerations
- Surgical consideration
- Select system and sound processor
- Step 5: Refer to an ENT specialist for a consultation or proceed with fit non-surgically
Step One: Candidate Criteria
The first step is to determine patients who can benefit from a bone conduction system, and which ones might be better off with a different solution. Before evaluating a candidate’s hearing, the candidate should feel the need for treatment. The patient may be of any age, although today’s focus is on the adult SSD candidate. These SSD patients may have specific expectations due to their type of hearing loss, and it is important to ensure their specific goals for hearing treatment can be met with a Baha System.
There are three areas to consider when determining candidate criteria: patient characteristics, patients with certain existing conditions, and patient attitude and history (Figure 4).
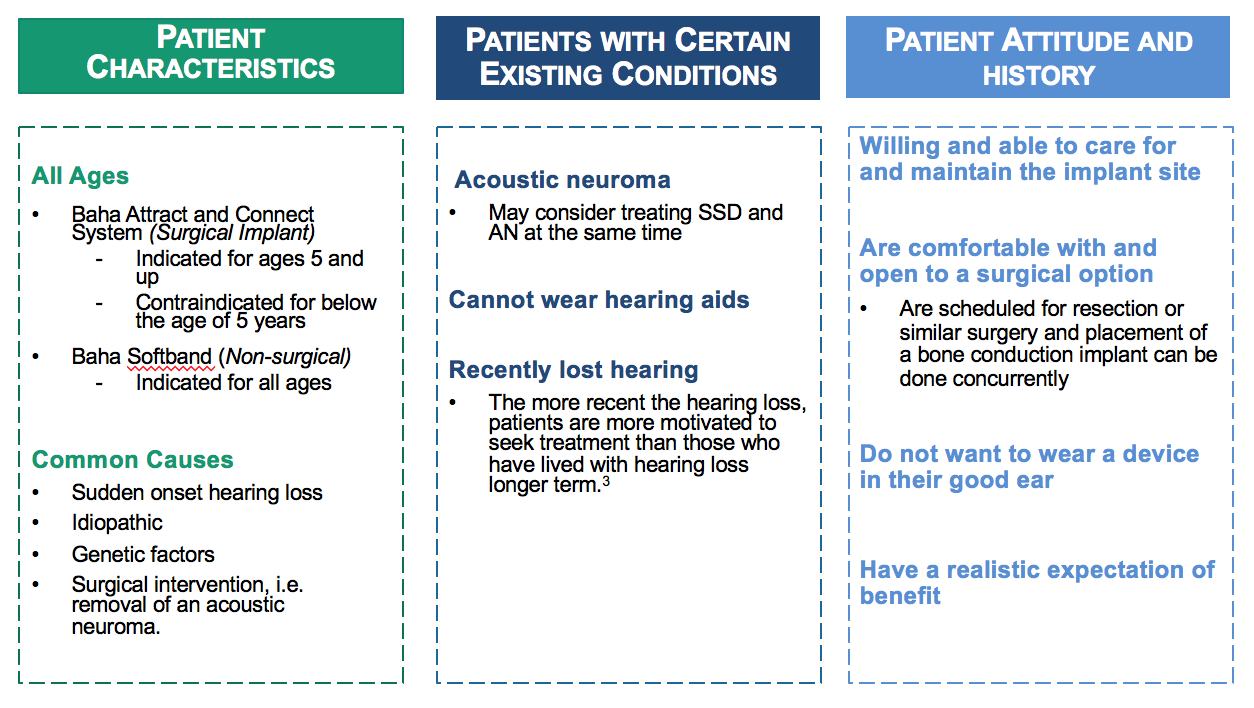
Figure 4. Determining candidate criteria.
Patient characteristics. The Baha Connect and Attract System (surgical implant) are contraindicated for anyone under five. However, we do have non-surgical options (softband) that are indicated for any age. Those connection points are the same, meaning you can use the Baha 5, the Power or the Superpower on any one of those connection points, whether it's Attract, Connect or Softband. Some of the common causes of SSD are sudden onset hearing loss, genetic factors, idiopathic causes and surgically related causes (such as removal of an acoustic neuroma).
Patients with certain existing conditions. I'd like to focus in particular on acoustic neuroma. In the past, there have been efforts to treat the acoustic neuroma, and install the implant at the same time. This is because once that acoustic neuroma is removed, hearing in that ear is no longer possible. Patients have that option to "kill two birds with one stone," so they can quickly get back into sound with the bone anchored implant.
Patient attitude and history. Is the patient willing and able to take care of the implant site? Care and maintenance is very important, particularly with the Connect or any sort of abutment style device implant. Are they comfortable with and open to a surgical option? Are they opposed to wearing a device in their good ear? Do they have realistic expectations of the benefits?
Step Two: Audiometric Testing
In addition to the audiological threshold criteria, protocol for speech testing is recommended to help objectively measure how clearly people can understand speech, with amplification and without (Figure 5). While pure tone thresholds are used to determine candidacy and gauge improvement in hearing levels, these measures have been demonstrated to be poor predictors of performance in background noise. The speech test material can be delivered through an audiometer via the bone conductor that is placed appropriately on the adult. To determine the presentation level, add 30 dB to the pure tone average, and increase by 15 dB until close to 100% is achieved on AB word test. Again, looking at the good ear is important in understanding an SSD patient.
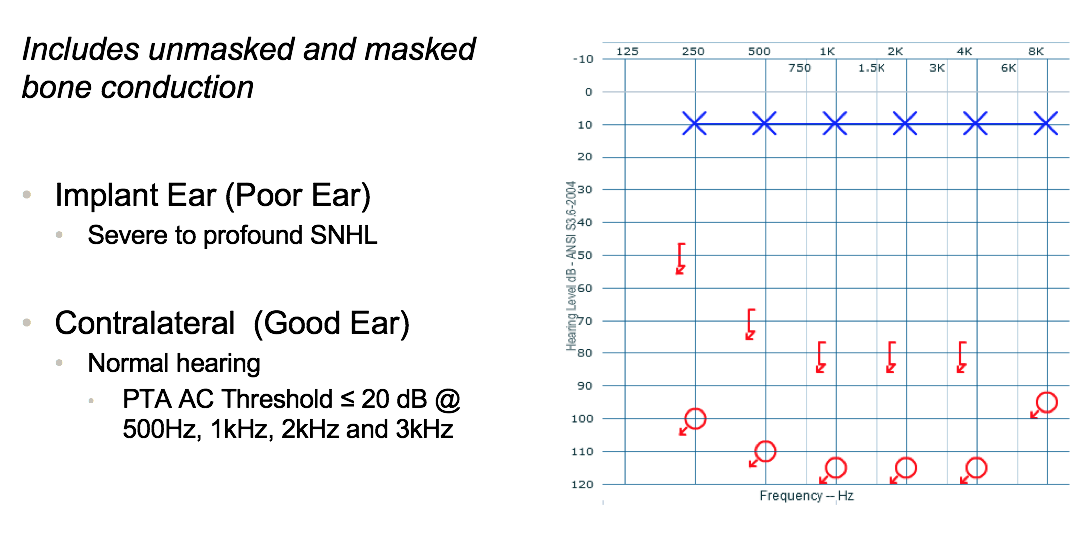
Figure 5. Audiometric testing.
Step Three: Clinical Benefit Evaluation
Cochlear recommends the use of the following tests to help evaluate the benefit: QuickSin, HINT, or AZ Bio. Test two situations to help determine individual benefit: unaided condition and an aided condition (using a Softband). It's important to test speech perception ability with the Baha System, as compared to an unaided condition. The difference in the signal-to-noise ratio between these two situations is a good predictor of individual benefit: the bigger the difference between aided and unaided, the more benefit can be expected from a Baha. The demonstration can be done using the Softband to show what it is like to have a Baha bone conduction processor on your head, very similar to what you could expect from Attract. However, the patient should expect better sound transmission using a Baha Connect System due to the penetration, and the direct bone stimulation. With Attract or non-surgical options (like Softband), there is soft tissue and transcranial attenuation, which may result in a 10-15 dB attenuation. Further information about hearing in noise testing to evaluate clinical benefit can be found in the course handout.
Step Four: Counsel the Candidate
Fitting Considerations. Practical points to consider include:
- Hearing Expectations: Are they choosing the correct power level? For example, what if they want an Attract, but they need a Connect? It is important to manage their expectations.
- Cosmetics: Are they okay with having something penetrating the skin (i.e., with Connect)?
- Hygiene: Are they capable of cleaning their site thoroughly effectively?
- Dexterity: Do they have dexterity issues? Will they be able to take the devices on and off? Will they be able to remove and replace the sound processor magnet, the software pads, and the processor itself?
- Sporting Activities/Head Gear: In the case of younger individuals, what are their sporting activities? What's their lifestyle like? Will they require head gear?
- Radiation/ MRIs
Surgical Considerations. Some typical surgical considerations to discuss include:
- Routine outpatient procedure: Are they comfortable with an outpatient procedure? How are they in general with surgical needs and expectations?
- General anesthesia: Are they okay being under general anesthesia? Are there any contraindications for them being under anesthesia?
- Established treatment option +40 years
Cochlear has published a guidebook titled "What to Expect at Surgery/Activation." It's very thorough with regard to procedure details, and also comprehensive in terms of assuaging patient fears. It is useful to help counsel patients on what the surgery is like, the typical procedure duration, and how the device is activated, among other information.
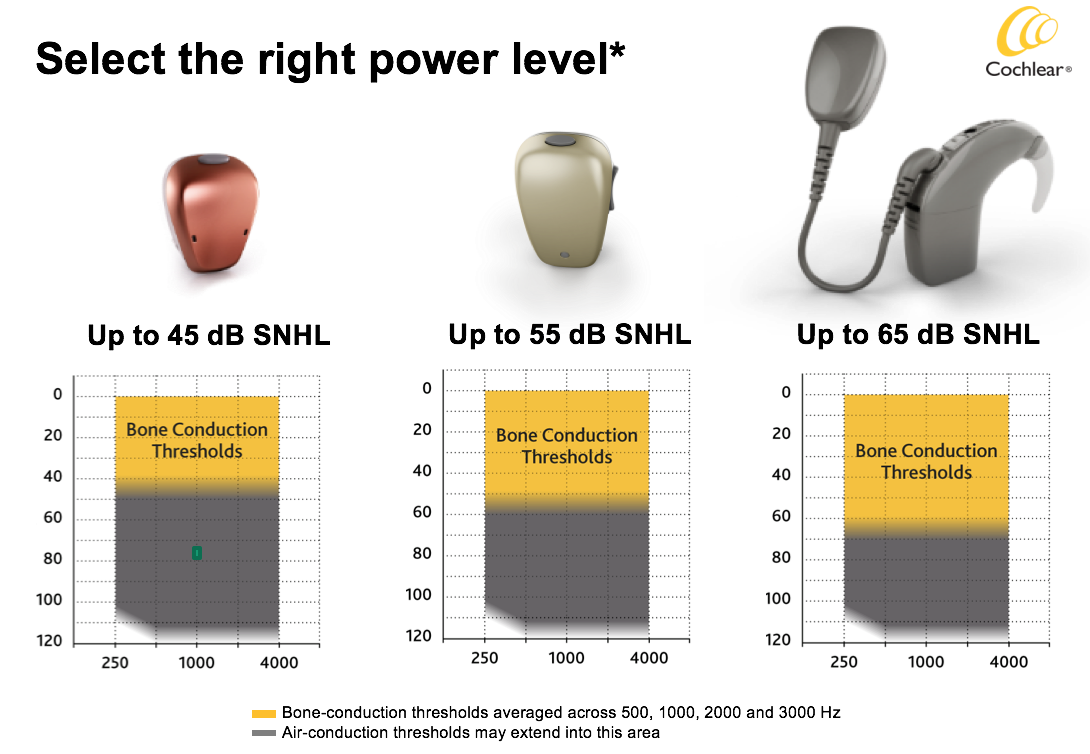
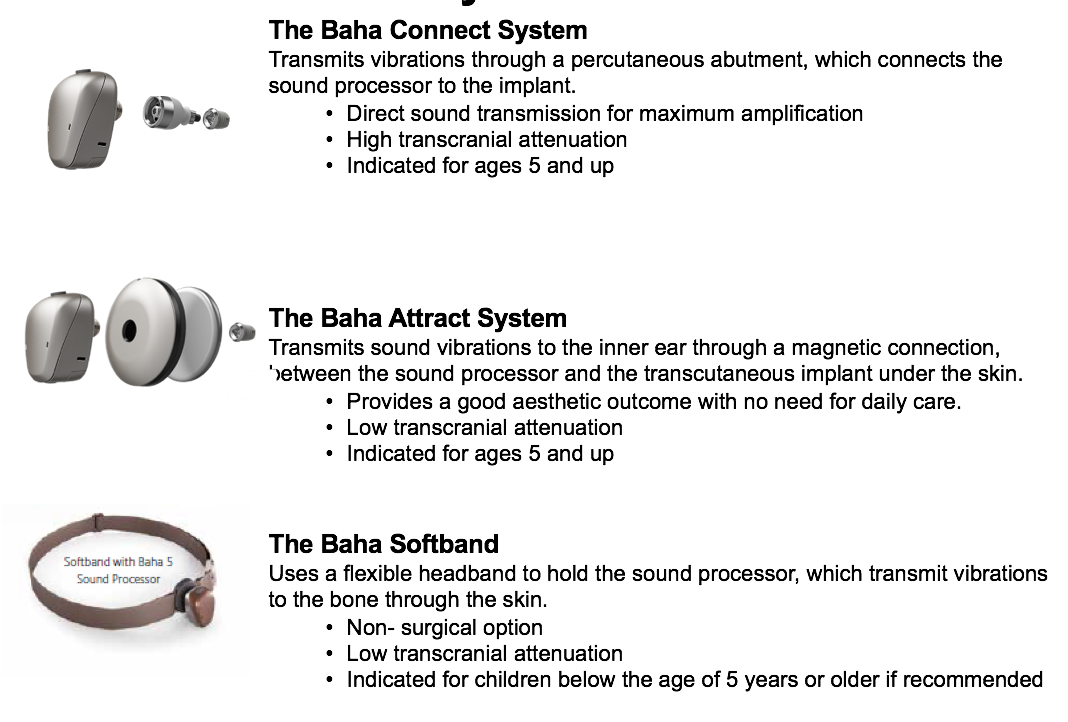
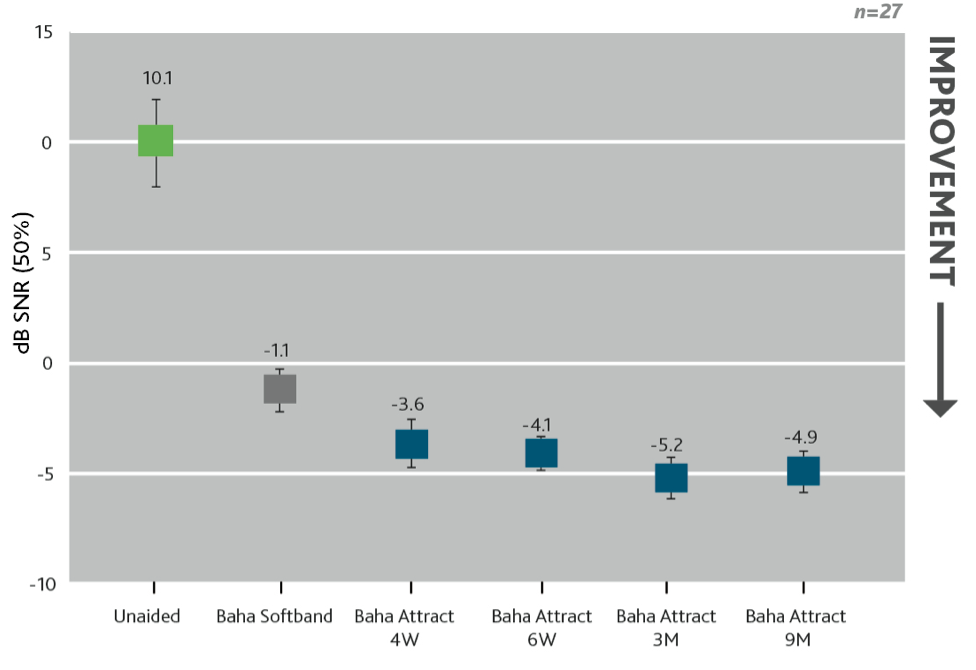
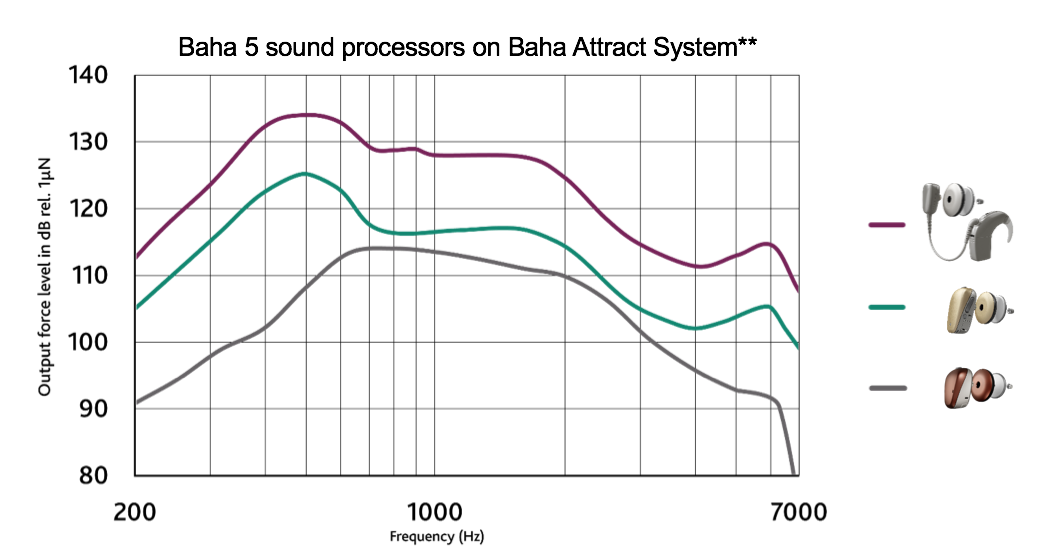
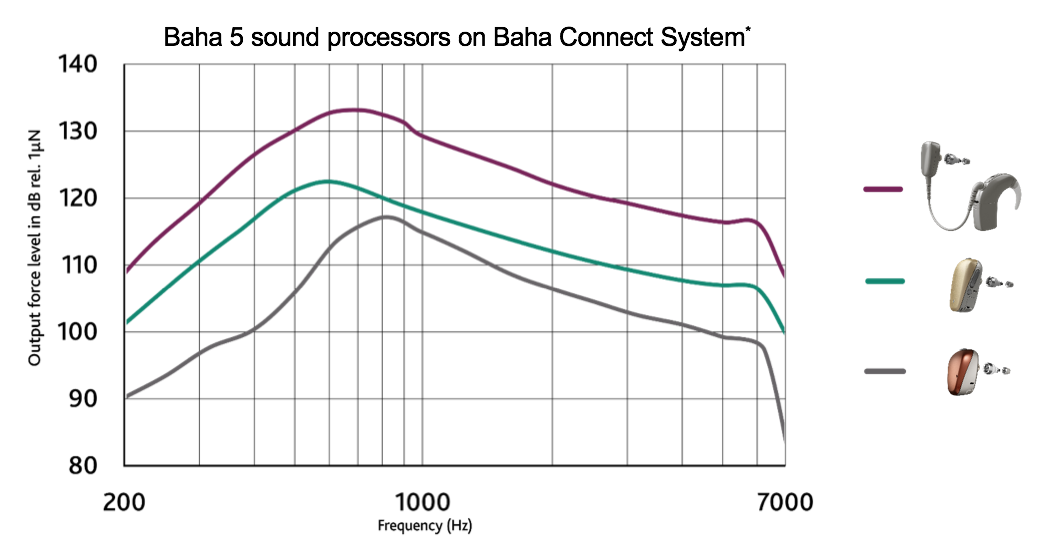
SSD Fitting Scenarios. There is no particular SSD sound processor, especially now that people are fitting SSD in mild to moderate hearing loss on contralateral ears. However, if you are fitting an SSD patient on a Softband or a Baha Attract, you might need a power processor to overcome the transcranial attenuation and soft tissue attenuation (Figure 11). Pure SSD on a Connect System essentially means it could be managed with a Baha 5. Occasionally, you'll come across high transcranial attenuation and need more power, but often a Baha 5 is enough.
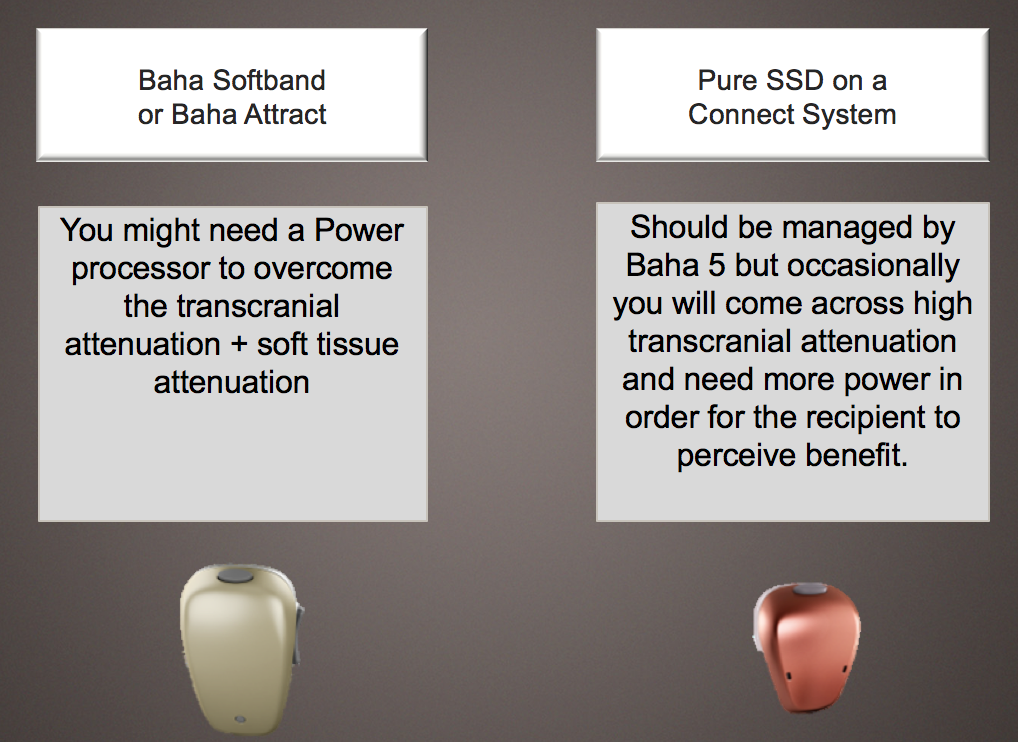
Figure 11. SSD fitting scenarios.
Attenuation is measured by comparing BC Direct and BC Unmasked thresholds. You should be able to tell if someone has high transcranial attenuation pre-implant when you fit them on a Softband. That's why it's so important to conduct a Softband trial for these patients. It not only benefits the patient, but it also helps you so you can do some objective testing and understand what that device can and cannot do. In my opinion, I believe the Baha 5 is sufficient for SSD, because you're not trying to overcome a conductive component; it's a sensorineural component that's involved.
Overview of Suggested Evaluation Process. Figure 12 shows an overview and flow chart of the suggested evaluation process for candidates with SSD. First, you take BC thresholds within fitting range of that Baha sound processor, you perform the BC Direct measurement with the Baha sound processor on a Softband, and do the BC Direct thresholds. At that point, evaluate whether they are in fitting range of the Baha SP. If the answer is yes, you'll finalize that fitting, perform testing again, and ask if the patient is satisfied. If they are satisfied, it is appropriate to think about an Attract System. If the answer is no, you might need to switch to a more powerful processor. Again, go back to that fitting and testing, and if they're happy, they could consider doing an Attract. Let's assume that you start with a Baha 5 and move to a Baha 5 Power; you could still consider an Attract at that time. Then use the Softband as a nice proxy for the Baha 5. If not, then consider all of the important factors associated with the patient's lifestyle for a Connect System.
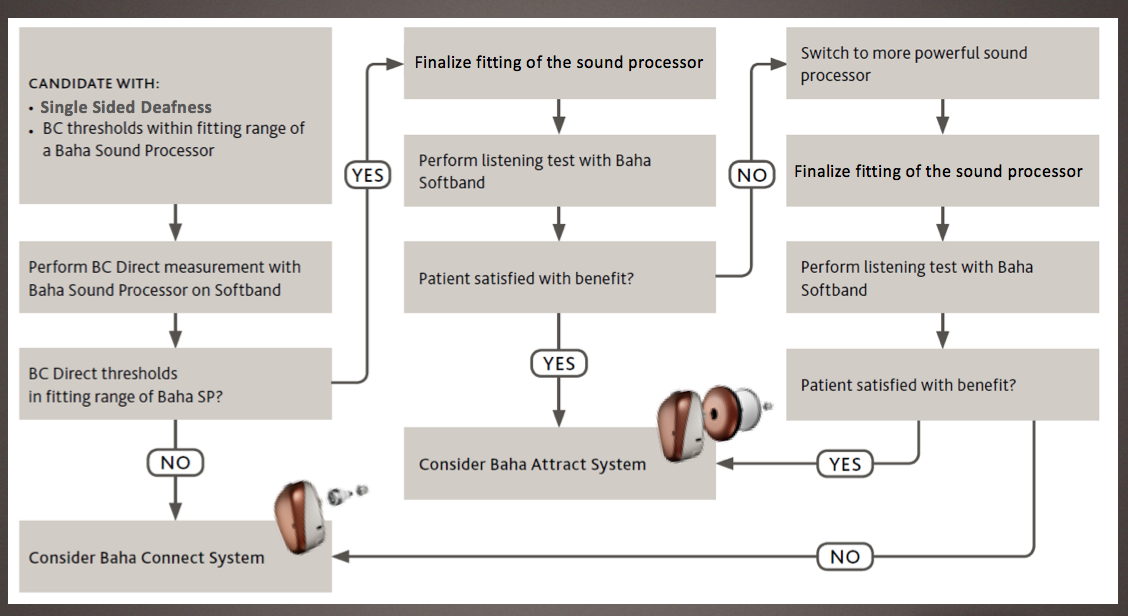
Figure 12. Overview of suggested evaluation process.
Contraindications. There are five contraindications to consider, where the implantation of Baha would not be recommended:
- Poor bone quality or thickness (e.g., osteoporosis): If the bone quality is not good, or it is not thick enough to hold the implant, you run the risk of having that implant not fit properly, as well as poor osseointegration. The surgeon will be able to assess whether or not they're a good candidate, based on a number of bone quality concerns.
- Poor hygiene (if considering Connect): The Connect System requires more after care than the magnet, because it sticks through the skin. We recommend wipes and keeping those abutments nice and clean.
- Unrealistic expectations (particularly with SSD): Is this going to restore my hearing in my dead ear? The answer is no: the cochlea is no longer functioning and there is sensorineural loss. Could it lift the Head Shadow Effect? Possibly. Could it help with lateralization? Sometimes. Is it going to restore full localization? Absolutely not. You want to make sure the patient has a clear understanding of what it can and cannot do.
- Medical conditions affecting bone and skin growth: There are lot of those folks who have keloid scars, or other conditions that might affect how the skin overgrows a Connect, in particular.
- Age (contraindicated in children below the age of 5): The age of the patient is a factor. Right now, the surgical options are contraindicated for children under the age of five.
Step Five: Refer to an ENT Specialist for a Consultation or Proceed with Non-Surgical Fitting
If your SSD patient meets candidate criteria outlined in Steps 1-4, your next step is to refer your patient to an ENT specialist for a consultation. You may work in offices where the implanting surgeon and others refer out. Either way, you can certainly allow your patients to take home a demonstration, if that's your office's preference. If your patient does not want to proceed with surgery, but does find value from the demonstration, consider fitting a Baha sound processor non-surgically and reevaluate over time.
SSD Case Studies
Now, I would like to go through a few case studies to talk about how these learnings can be applied in your practice.
Case Study: Steve
Steve is a 38-year-old man with sudden SSD of unknown etiology three years ago. He sings in a 1940's tribute band and wears suits and horn-rimmed glasses every day. He has been using a CROS aid, but he does not like wearing it with his glasses. With the CROS aid, he feels that his good ear is plugged, especially when he's trying to follow his bandmates and keep on time with his music.
According to Steve's left and right audiograms, this does appear to be a classic case of SSD (Figure 13).
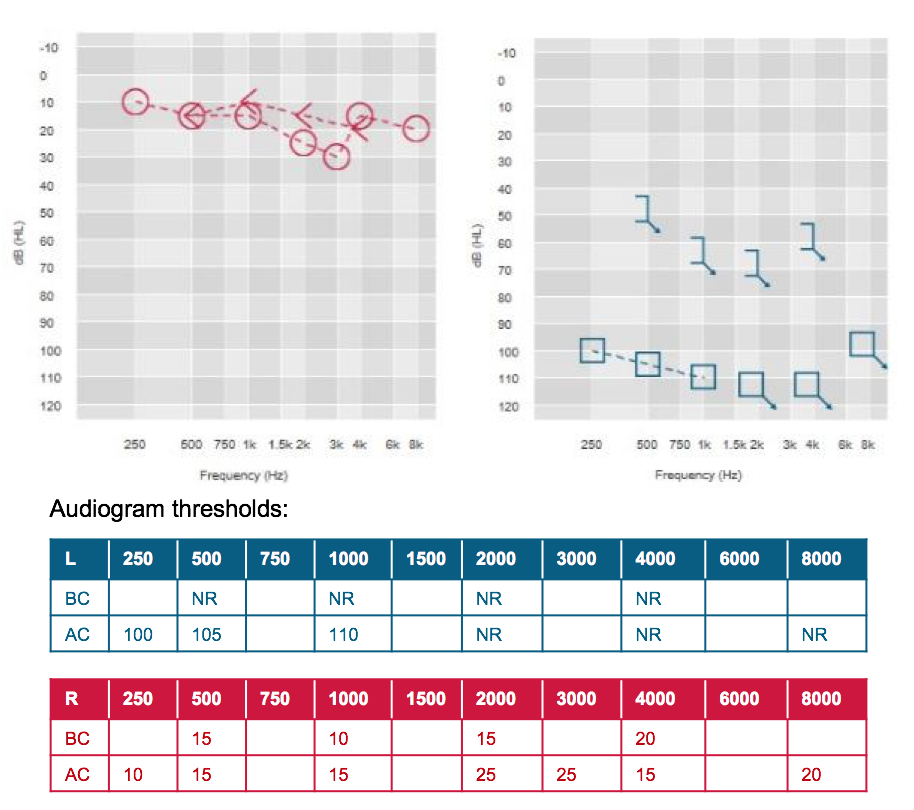
Figure 13. Steve's audiogram thresholds.
Following a successful trial in the clinic, Steve elected to move forward with a Baha Connect in the left ear. He successfully uses his Baha every day, and reports that it's so comfortable, he sometimes forgets he's wearing it. In Figure 14, you can see Steve's unaided condition, as compared to results from the Softband trial, and finally the abutment post-op.
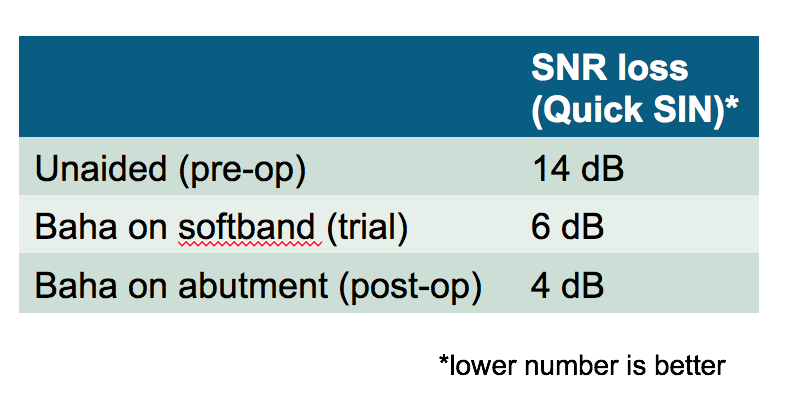
Figure 14. Steve's outcome with Baha Connect in the left ear.
Steve commented, "I love using the Baha to talk on my iPhone. I didn't expect that it would be so clear to use on the phone." Patients love the Made for iPhone connectivity with any of the devices in our Baha 5 line.
Case Study: Lia
Lia is a 62-year-old woman with a congenital hearing loss in the right ear. Recently, she has noticed some loss of hearing in her good ear, and she is struggling to communicate at work. Lia is a florist who owns her own shop. She's very active and does not plan on retiring any time soon. Lia has not tried any previous treatment options for her hearing loss.
One thing that we didn't discuss is the difference between the prevalent and incident population. People in the incident population are those who experience sudden loss. People in the prevalent population are walking around unaided, having never received treatment for their hearing loss. They believe that one ear is good enough, or they never felt they had a deficit. I'd like to argue that at some point, those in the prevalent population are important to get in the door and have them at least test a device, so that they understand what they're missing.
Figure 15 shows Lia's left and right audiograms in the unaided condition.
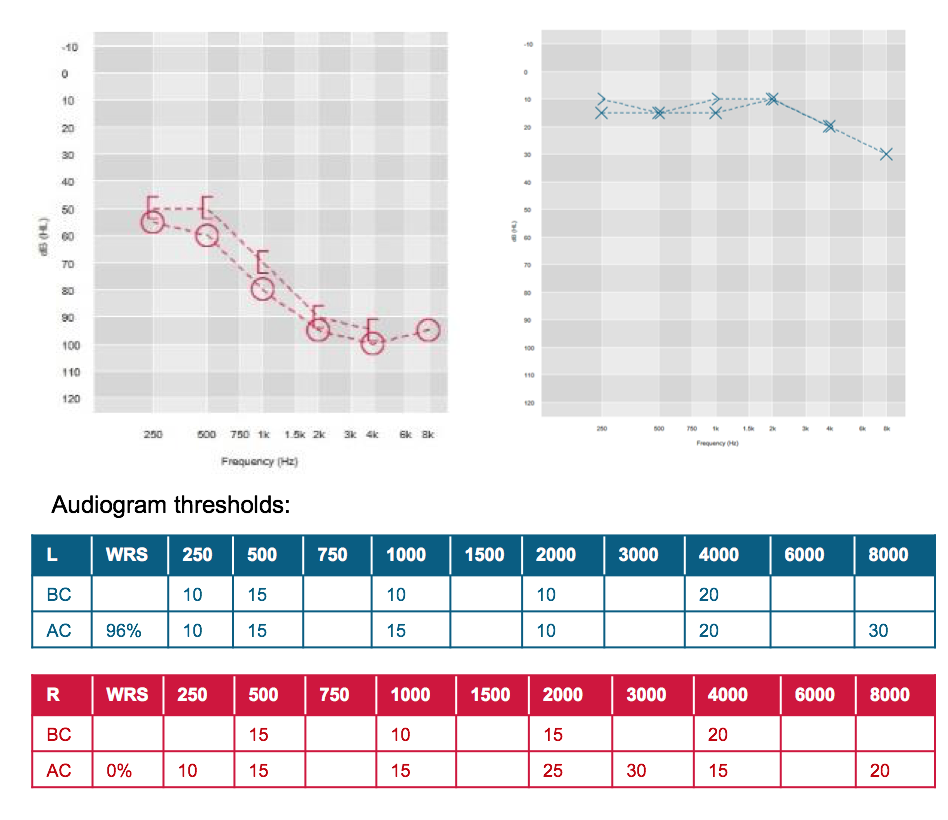
Figure 15. Lia's audiogram thresholds.
Lia's clinician discussed treatment options with her and she chose to try out the Baha first. She loved the sound of the Baha 5 Power on the Softband and elected to proceed with the Connect. Lia uses her Baha daily, and especially likes using the Mini Mic, another wireless device that does not need a dongle. It's just True Wireless between her sound processor and her device at work with her colleagues.
In Figure 16, you can see Lia's her unaided condition from a pre-op standpoint, her trial with the Softband and her improvement on the abutment. She commented, "I barely notice my Baha, but my employees at work definitely notice if I don't have it on!" This quote is a great commentary on how much Lia may have been missing in the unaided condition.
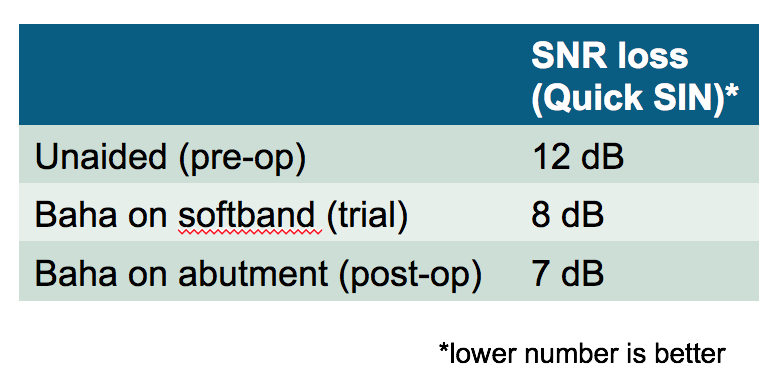
Figure 16. Lia's outcome.
Summary and Conclusion
In summary, some of the benefits of the Baha System that your patients with SSD may experience include:
- Improved sound quality due to direct bone conduction
- An enhanced sense of directionality due to increased sensation of sound on side with loss
- Improved speech understanding in noisy environments
- Long-term patient satisfaction and hearing benefits
- Ability to try before they buy
Furthermore, additional benefits of Baha, as compared to two of the biggest complaints we hear related to CROS hearing aids, are:
- No need to wear hearing devices on both ears
- No occlusion of the hearing ear
Questions and Answers
References
Citation
Hurley, P. (2017, December). Hearing from the other side: Understanding the candidacy for SSD and treatment options. AudiologyOnline, Article 21327. Retrieved from www.audiologyonline.com


