Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials here.
Welcome to today’s presentation, Reimbursement and Bone Anchored Hearing Systems. I’m Carrie Hart, the Director of Reimbursement for Oticon Medical. I’m happy to be here today to review some of the fundamentals of healthcare reimbursement and how they specifically relate to bone anchored hearing systems, like Oticon’s Ponto system.
Today’s agenda will include a review of the three fundamentals of reimbursement: coding, coverage and payments. We’ll dive into specifics, but given our time constraints, you’ll find that we’ll spend the most time specifically reviewing the current Medicare payment rates. At the end of the allotted time, we will touch on the concepts and how they all roll together to help you better understand what is needed to efficiently have a bone anchored hearing program.
As we get started, it is important to mention three terms that you will see throughout the day: coding, coverage and payment. Sometimes they are referred to as the keys, the elements, or the building blocks of reimbursement. Individually they are all very important, but together they are the basis of understanding reimbursement. We’ll go into further detail as we move forward, but to quickly introduce you to these concepts, coding refers to a group of systems that are used to identify services, devices, drugs, and even patient diagnoses. Coverage refers to the circumstances under which a payer will reimburse for a given test or procedure. It’s based on contract provisions and medical necessity. Payment, simply enough, is the amount that is actually reimbursed to the healthcare providers for their provision of services. There are various methodologies in place for calculating that amount of payment.
Coding
Let’s first review coding. In the United States (US), over 5 billion claims a year are processed for payment. To ensure that claims are processed orderly and consistently, there is a need for standardized coding. We’re not going to go through the entire list of codes today, but as noted in our course title, today we’re reviewing reimbursement as it relates to bone anchored hearing systems. There are three applicable coding systems.
The first is the CPT, and that is an acronym for Current Procedural Terminology. These codes are used to describe the medical, surgical, and diagnostic services. For today’s purpose, these codes would be used to identify the surgical procedure. Next are the HCPCS codes, or an acronym for Healthcare Common Procedure Coding System. They would be used to describe products, supplies, drugs and durable medical equipment (DME) items. Again, to relate this back to our product, these would be used to identify the device; including the processor, whether at the time of surgery for use on a softband or even a replacement product. Finally, we have the ICD-9-CM diagnosis codes, or International Classification of Diseases, 9th Revision, Clinical Modification. These codes are used to describe the patient’s primary, secondary, and any additional diagnoses that prompted the treatment or visit. As with all codes, it’s really important to be specific, but especially with these diagnosis codes, because you can use multiple codes to describe what is going on with the patient and what prompted that visit.
As we move a move forward, I wanted to make you aware that CPT is a registered trademark of the American Medical Association (AMA). The AMA is responsible for publishing a yearly listing of comprehensive codes and all of their descriptions. They are responsible for making decisions about adding codes to the list as well. Not to confuse matters, but the CPT codes are also sometimes referred to as Level I HCPCS codes. You’ll always be able to identify a CPT code because they have five numeric digits.
CPT
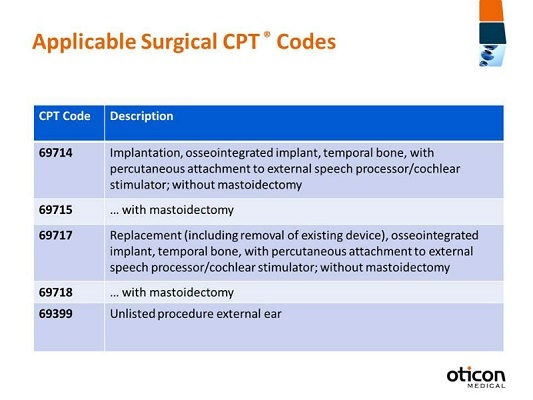
When we look at the CPT codes that are applicable to bone anchored hearing systems (Figure 1), you’ll see that they’ve been created to describe the actual surgical procedure. 69714 is the most commonly billed code as it relates to bone anchored hearing. The code’s description reads: implantation, osseointegrated implant, temporal bone, with percutaneous attachment to external speech processor, cochlear stimulator without mastoidectomy. Remember, this is for the procedure, so although the device is mentioned in the description, this code does not include the device. This is only to identify the procedure. Also note that 69714 is used to identify when a mastoidectomy is not performed. If a physician were to do this procedure with a mastoidectomy also, 69715 would be used.
Figure 1. Applicable surgical CPT codes.
Less commonly billed are the next two codes, 69717 and 69718, as these codes describe a scenario where a physician would need to remove and replace the patient’s implant or abutment. Again, you’ll see the code descriptors have ‘without a mastoidectomy’ as well as ‘with a mastoidectomy’ (Figure 1). I have also included a miscellaneous code, 69399. The miscellaneous codes don’t have very specific descriptions. This one says, “unlisted procedure, external ear,” but the reason that I’ve included this is because this code is used most often to identify when a physician has needed to make a revision or to change a patient’s abutment to one that is longer or even angled. When one of these codes would be used, it would require that more documentation and chart notes be submitted with it so that the payer would understand what was actually done.
HCPCS
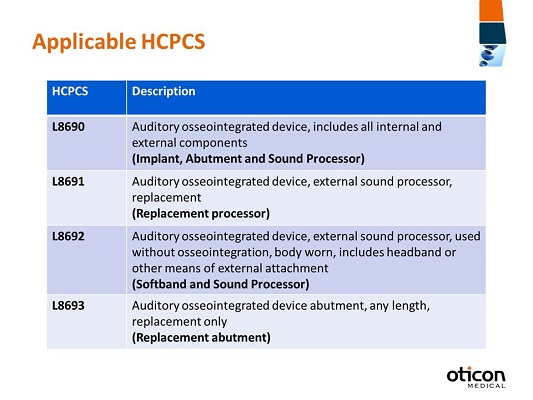
HCPCS is an acronym for Healthcare Common Procedure Coding System. The HCPCS is actually divided into two systems: Level I, which are the CPT codes, and Level II, which is what we commonly refer to as HCPCS codes. As we move forward in this presentation, whenever I refer to HCPCS codes, I am talking about the Level II codes. HCPCS codes are developed and maintained for the Centers for Medicare and Medicaid services, which is also known as CMS, or simply Medicare. On a yearly calendar, they make decisions whether or not to make updates to this coding system, which they then publish. These codes are used primarily to identify products, supplies, and services that aren’t included in the CPT codes. Different from CPT codes, HCPCS codes are going to be alpha-numeric, so they have one letter followed by four digits. The letter has significance; it actually corresponds to a category of coding. Prosthetic devices actually start with the letter L. I’ve listed out for you the applicable HCPCS codes for bone anchored hearing (Figure 2). The first is L8690, and that description is auditory osseointegrated device, includes all internal and external components. That is the implant, the abutment, and the sound processor. This code would be billed at the time of surgery.
Figure 2. Applicable HCPCS codes for bone-anchored hearing systems.
Next, L8691 is the osseointegrated device, external sound processor replacement. Again, I noted in bold that this is the replacement processor. It’s important to remember that there are a variety of sound processors available, but the coding is not brand-specific or item-specific, in that there is only one code regardless of which sound processor is prescribed for use.
Next we have L8692, which is auditory osseointegrated device, external sound processor, used without osseointegration, body worn, includes headband or other means of external attachment. This code is most commonly used for children as they are prescribed to use the sound processor on a softband. It can also be used for a headband for folks who are waiting for surgery and are wearing it on a headband externally, but it’s most commonly used for kids who cannot yet have surgery based on our FDA-cleared indications or for other reasons. It’s always important to remember that this code is not just for the sound processor; it’s for the sound processor and the softband or the headband.
Finally is L8693, and that is the osseointegrated device abutment, any length, replacement only. This is only to identify when a new abutment is placed. As I mentioned earlier, when we talked about the CPT codes, there may be a need for some patients to replace their abutment with one that is longer or even angled, and this would be the code to identify only the device. For example, Oticon offers a variety of abutment sizes, 6, 9, 12 millimeter and angled, but there’s one code for all the different sizes.
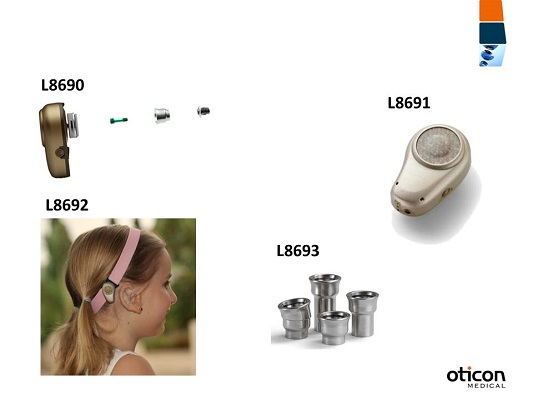
I’m a visual person so I put together Figure 3 because instead of just looking at lists of codes, I think it’s nice to be able to have a visual representation of what the product looks like along with the code. In the first image of L8690, you’ll see the implant, the abutment, the surgical screw that’s used, and then the sound processor. In L8691, this image is of one sound processor. Our company actually has three from which to choose, the Ponto, the Ponto Pro, and a Ponto Pro Power, but remember the same code is used regardless of processor or brand. Then L8692, this sweet little girl is wearing a pink softband as well as the sound processor, and then L8693 is for a replacement abutment.
Figure 3. Picture view of HCPCS codes and their associated product.
ICD-9-CM
Finally we go to the ICD codes or the International Classification of Diseases code set. The current coding system being used right now is the ICD-9 code set, and these are all based on the World Health Organization’s ninth revision. That’s important to know that the World Health Organization has this consistent coding set that is used globally for reporting on mortality and morbidity. We are actually on the ICD-9 set right now. There’s going to be a transition to ICD-10 soon that I will talk about in a minute, but what’s important to know is that we currently are still using the ICD-9 codes. They are used to identify or report a patient diagnosis. They are also used to report inpatient procedures, but for the purposes of our presentation today, we don’t need to focus on the inpatient procedures, as bone anchored hearing solutions are always surgically placed on an outpatient basis.
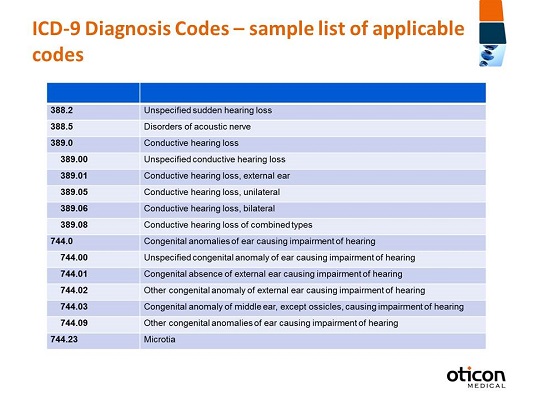
When it comes to these codes, although they’re based on the World Health Organization coding system, it’s actually the National Center for Health Statistics (NCHS) and Medicare that are the US Government Agencies responsible for any changes and modifications. Figure 4 is a sample list. It’s obviously not all-inclusive, but it is a list of potential ICD-9 codes which could be used to identify a patient who may be a candidate for a bone anchored hearing solution. As I mentioned earlier, specificity is of great importance here. You can have codes that describe conductive hearing loss, but as you move down they get more specific. If there are any congenital anomalies of the ear, you can be more specific with what those anomalies actually might be.
Figure 4. Sample list of applicable ICD-9 codes of a candidate for a bone-anchored hearing system.
The transition from ICD-9 to ICD-10 will be interesting. Currently there are 17,000 codes in the ICD-9 system. We are moving to the ICD-10 codes, which incorporate approximately 141,000 codes. There are going to be a lot more specific ICD-10 codes, and many of the ICD-9 codes that are currently being used are actually going to map to multiple ICD-10 codes. This transition is required for everybody who is covered under HIPAA (Health Insurance Portability and Accountability Act), so it’s very important to be aware of these changes. The compliance deadline is October 1, 2014, which might seems like it’s a ways out there, but as we all know, time seems to go by very quickly. Medicare is already publishing quite a bit of good information on their Web site, and I highly recommend that you visit it (https://cms.gov/Medicare/Coding/ICD10/index.html). They have a lot of good information including frequently asked questions on how you can prepare, as well as general equivalence mappings so you can see how these ICD-9 codes are going to transition to the ICD-10 system. It’s important to already start looking at your billing software, talking to your software vendors, and even reviewing your payer contracts for how there might be any implications. Again, that deadline is October 1, 2014 so any claims on or after that date need to be using the new coding system.
Coverage
We’ve reviewed the applicable coding systems; now let’s move onto coverage. Coverage is a circumstance under which a payer will reimburse a provider for services, procedures, devices, and drugs. It’s important to remember that coverage is an agreement. Decisions to cover things like diagnostic testing, procedures or services are based on this agreement that’s in place. It’s all outlined in the patient’s certificate of benefits. When we talk about coverage decisions, they’re going to be based on these contract provisions and something called medical necessity, which I’m sure we’re all familiar with. What’s really important to know is that the patient needs to understand what their allowed benefits might be as they are outlined in their agreements. The patient or the member should always get a certificate of coverage or a certificate of benefits, whether they’re on an individual plan or covered under their employer’s plan.
This document outlines any specific exclusions there might be from benefits, such as cosmetic surgery, which is typically an exclusion. There might be specific riders, as well. There might be some additional benefits that the member has, like hearing aid coverage. These documents also outline any limitations that might exist. For example, a member might be allowed to have a specific number of physical therapy appointments or chiropractic visits. What’s important about this document when we talk about bone anchored hearing is that it should serve to define different meanings. For example, what is a prosthetic device? When is a prosthetic device covered? Are there any limitations to prosthetic coverage? You’ll see as we move forward that is very important when we talk about bone anchored hearing systems.
When we talk about coverage, we’re not just talking about the certificate of coverage. We’re also talking about coverage policies that a payer might have in place. A coverage policy is really how a payer outlines how the member must meet certain clinical or medical requirements. They define under what circumstances they will cover something. Does a patient need to have a certain diagnosis or certain test results? It’s always important to remember that you can’t make blanket statements. It’s hard to say X-Y- Z payer always covers a certain device because there’s going to be a variation by the different plans that are offered by the same payer. It could be driven by the employer plan, the individual plan, whether or not it’s an HMO or a PPO, et cetera.
We talked a little bit about coverage, and we mentioned medical necessity. Proof of medical necessity or proof that a covered member meets requirements that are set forth in a clinical policy is very important. As I noted before, that typically means that a patient needs to meet certain requirements that the insurance company has laid out, like a particular diagnosis or test result.
When you talk about medical necessity, what’s really important to understand is that these payers are looking at standards. They’re looking at the fact that this treatment must meet acceptable standards of medical practice, so they don’t want something that’s considered experimental or investigational. They want it to be something that’s considered reasonable and necessary; those are sort of the buzz words when you talk about medical necessity.
Back in the early 2000’s, bone anchored devices as a treatment was new, and we would run into payers denying coverage, telling us that it was considered experimental or investigational. As time has passed and the technology has been implanted in more patients and there have been more and more studies published with further evidence showing that the device is safe and that is effective, we don’t see this as much. It has been cleared by the FDA since 1996, so I think there’s a lot of good evidence for us to show payers that the treatment with bone-anchored hearing is very reasonable; it is necessary.
Medicare
In talking about coverage in general, I think it’s important to move into talking about specific coverage that is in place with Medicare. Why Medicare? Medicare is the body that governmental payers and private payers look to before or during their decision-making on whether or not to cover something. They also look to Medicare in their payment decisions. As we all know, Medicare doesn’t make decisions lightly. Many may say that they don’t have to follow Medicare, but in actuality they do look at them as having set the precedent because Medicare has gone through a lot of due diligence to make any decisions. As we talk specifically about Medicare coverage for bone anchored hearing devices, it’s important to point out that since Medicare was established in 1965, they have excluded coverage for hearing aids. In their benefit policy manual, they outline general exclusions from coverage and they note that no payment may be made for expenses incurred for hearing aids.
However, in November 2005, Medicare actually modified the hearing aid definition. In doing so, they address exclusions for hearing aids, but they have also excluded certain implanted devices from the category of hearing aid, making those covered devices. What they did with regard to bone anchored hearing was define osseointegrated implants as prosthetics. Certain devices that replace the function of the middle ear or cochlea are considered prosthetics by their definition. Prosthetics are deemed medically necessary when hearing loss or other anatomical anomalies make traditional hearing aids inappropriate. The two most important things about their definition are replacing the function and as prosthetic devices. It’s very important to understand that is how Medicare is covering the bone anchored devices. Even as we go further into that definition, you’ll see that Medicare specifically calls out the following prosthetic devices: cochlear implants, auditory brainstem implants, and osseointegrated implants. Those are devices implanted in the skull that replace the function of the middle ear, and they provide mechanical energy to the cochlea via a mechanical transducer.
As I noted before, other payers look to Medicare. So now that we have Medicare patients who are able to have the device implanted, we have other payers who can look to Medicare for coverage, including Medicaid. Often times you’re going to find that the state Medicaid plans are going to look to what Medicare does. Medicare has pulled these devices out from the hearing aid definition. However, that is specific to devices that are implanted. It’s important to note that L8692, which again is the code that used to identify the softband and the sound processor or headband with a sound processor, would not be covered by Medicare because it does not meet this definition. It does not meet the definition of a prosthetic according to Medicare.
I think when we talk about Medicare coverage it’s important to talk about the fact that Medicare also will cover replacement sound processors. As I mentioned earlier, the device has been cleared by the FDA since 1996; it’s been on the market since then. More and more people have been implanted, and they’re finding that as some time has gone by, they may need or desire a replacement sound processor. Expenses for a replacement due to loss or irreparable damage might be reimbursed, but it’s based on the contractor’s judgment. Under irreparable damage they need to have a specific accident or a natural disaster, unfortunately like a flood, that they can present to Medicare to show that that is the reason they need a replacement. They wouldn’t need a physician’s order, but they would need to go to their local Medicare to obtain coverage and a replacement.
We move onto irreparable wear, which is day-to-day usage of the device, which then causes some deterioration because you’ve used it every day over time. This takes into consideration something that Medicare calls reasonable useful lifetime, which is going to be equated to about five years. If it’s been in continuous use by the patient, they can actually elect to obtain new equipment. The important thing to note is that it does require a physician order to get this replacement, because Medicare wants to understand and know that it’s still medically necessary. It’s still doing its job to treat the patient’s diagnosis or illness. I’d also like to note that during this five years, Medicare does cover repairs to the device.
Lastly, replacement coverage under Medicare exists when there is a change in the patient’s medical condition. If replacement is due to a change in the patient’s condition, it must be supported by the physician’s order. We talked before about how important medical necessity is. This is an instance where there must be an identifiable change in the patients’ condition that would warrant a replacement. They would require evidence via audiograms or other testing, as well as an understanding of the sound processor and how that would treat those changes.
Medicaid
When we talk about coverage, there’s Medicare, Medicaid, and private payers. Medicaid is funded jointly by the federal government and the states. It’s inherent in that name, Centers for Medicare and Medicaid services. Unfortunately, for our sake in trying to understand the coverage in place for bone anchored hearing, there’s going to be some variations in coverage because it is managed by each individual state. The states are going to make their own coverage decisions, and they will publish them and make them available for review. What we’ve seen in talking to our customers and patients and just in review of the policies that are out there is that there is quite a bit of variation. Sometimes there are no issues with having the surgery and the device covered. What we’ve also seen that we find quite confusing is that the surgery is sometimes indicated as being a covered procedure, but the device is not covered. So even if you are billing for the surgery and the device that would be implanted at the time of surgery, the surgery would be covered but not the device. We are working and trying to educate those state Medicaid plans about that scenario so that we can hopefully evoke some changes in those policies.
We have also seen certain states that do not cover the surgical procedure, but they will cover treatment for children with a softband and a sound processor. Sometimes that’s because that particular state may have mandates for hearing aid coverage, so they may cover it as a hearing aid. Other times they just have limitations where they will cover the hearing restoration for a younger patient but not an older patient. There are age restrictions in both treatment methodologies, too. Sometimes the surgery and device is only covered up until the age of 18 or 21.
To summarize, it’s very important if you identify a candidate to always check their benefits, always understand what coverage is in place, and what limitations or exclusions there are. I’d also like to encourage you as we move forward to get in touch with us when you run into these situations. As a manufacturer, we are very happy to help you whether it be contacting the Medicaid plan or to help make changes in these policies. We are currently working with one particular state that unfortunately had their coverage written so that even the softband and the sound processor were not covered until the age of 5. They had looked at our FDA clearance for surgical implantation, which is after the age of 5, and applied that also to the softband and sound processor. That’s currently being changed, which is wonderful, because then children from birth to age five will finally have access to the softband and sound processor. Please make us aware of any of these issues you might find in your local area.
Payment
We’ve reviewed coding coverage a bit; now let’s move onto payment. Payment is going to be the amount or the reimbursement that is paid to a healthcare professional or a facility for the provision of services. As I noted before, methodologies vary, and it’s important to understand not only the terms and conditions when you have a contract in place with a private payer, but it’s also important to understand what payment you are getting. With the governmental payers, which is what we’re going to move forward and talk more about, your payment methodology is set; it is what it is. But when you talk about private payers, payment is negotiable, so it’s really important as a provider to understand and evaluate what your costs are versus your reimbursement rates when you look at setting up a program and negotiating any contracts.
Medicare
Medicare makes payments in essentially two methods. One is the fee schedule, which is a listing of fees used by Medicare to pay doctors and other suppliers. It is essentially going to be a listing of codes and what the reimbursement rate is associated with that particular code. It’s also referred to as fee-for-service, because really it is getting paid for the service you provide and identify using the coding system. There’s also the prospective payment system. In the last several years, Medicare has looked at this and decided to go from being just a payer of claims, to adjudicating claims and sending out a check, to being a savvy purchaser of healthcare. The prospective payment system was developed where Medicare has a way of looking and establishing a predetermined, fixed amount of reimbursement. They look at a procedure and evaluate all the costs that are going to go into performing this procedure. They look at all the overhead and different factors that play into it, and they have one lump sum payment for it as a way of increasing efficiency at different healthcare providers. They know what they’re going to get paid and they need to be more efficient in how they provide that care. The payment amount is usually going to be based on the classification like an APC (Ambulatory Payment Classifications) or a DRG (diagnosis-related grouping). We’ll go into that a little bit further.
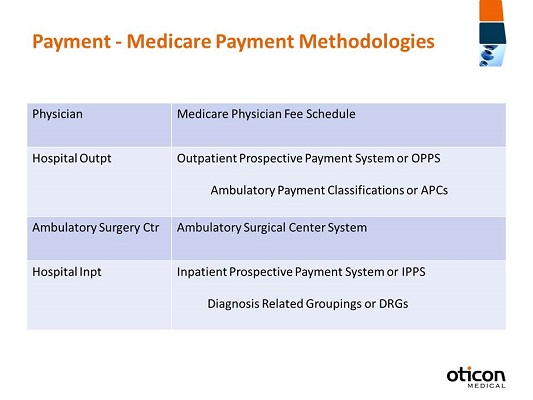
Figure 5 shows the different Medicare payment methodologies. As we said earlier, they pay physicians on the Medicare Physician Fee Schedule. For hospital outpatient, the system is called the Outpatient Perspective Payment System or OPPS, sometimes also know as HOPPS for Hospital Outpatient Perspective Payment System, but the payment classifications are called the Ambulatory Payment Classifications (APC). Ambulatory surgery centers (ASC) get paid on their own system, and hospital inpatient or Inpatient Perspective Payment System gets paid on diagnosis-related groupings or DRGs. This payment system is driven on what the patient’s diagnosis might be, so can see why it’s important to understand the ICD-9 transition to ICD-10, because the payment is going to be driven by those codes.
Figure 5. Medicare payment methodologies.
We’re focusing on the Medicare payment methodologies, but similar to coverage, other payers like Medicaid and private payers look to Medicare as setting a precedent. They may follow these same payment methodologies. Sometimes private payers pay a percentage of billed charges instead. Sometimes you’ll see that they pay a percentage of the Medicare fee schedule. In particular, when it comes to physician fee schedule payment, you might see where they contract to pay a percentage of that, like 125% of the Medicare fee schedule. It’s important to remember that Medicare doesn’t take these decisions on how they make payments lightly. They put a lot of thought into it. They have a lot of resources and other organizations that give input, so the decisions they make are looked at seriously by other payers.
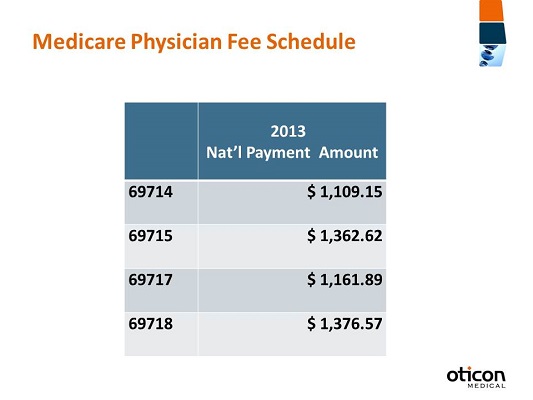
As we go specifically into the Medicare Physician Fee Schedule, Figure 6 shows the 2013 national payment amounts for the surgical codes for bone-anchored hearing. For 69714, the national amount is $1,109.15, and that’s going to be the most commonly billed code. This is the payment amount to the physician for their surgical time on this procedure. Remember that this fee schedule amount is going to be the national payment amount, and these are the total allowable amounts. This is what would be published by Medicare as the allowable payment. Any actual payment would be less. Any annual deductible or co-insurance is the patients’ responsibility.
Figure 6. National payment amounts for 2013 Medicare physician fee schedule.
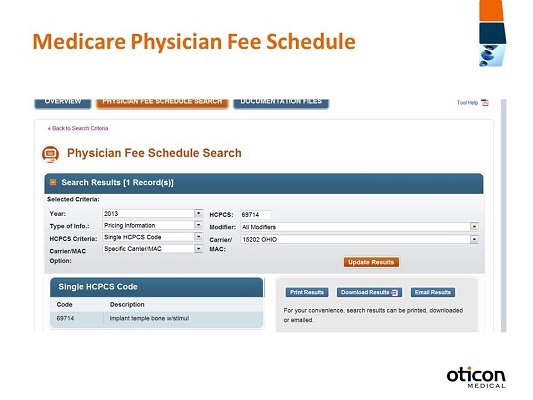
I wanted to show you how you can look this up. I gave you the national amount, and payment is typically going to vary based on geography or locality, so I want to give you an example of how you would look up your local fee schedule. If you go to the following Web page (https://www.cms.gov/apps/physician-fee-schedule/overview.aspx), you can see that you can start the search for the physician fee schedule look up; it’s a very nice tool that they have provided. Just agree to the different waivers; you’ll accept those. Now what we’re going to quickly do is look up one code (Figure 7).
Figure 7. Screen shot from the Physician Fee Schedule search portal.
We selected 2013 because that’s the fee schedule we’re interested in. We want to understand pricing information. We’re going to do a single code for today. As you’ll see, you have a choice between the national amount, a specific carrier or Medicare Administrative Contractor (MAC), and a specific locality. I’m going to do a locality, and I’m going to put in 69714 (Figure 7). You must select a modifier. I usually just choose all modifiers in case there is some sort of variation that comes up. Then we’re going to select our locality or carrier. I live in Ohio, so I’m going to choose Ohio down here at the bottom, but you have many choices based on your locality. Then submit by clicking Update Results.
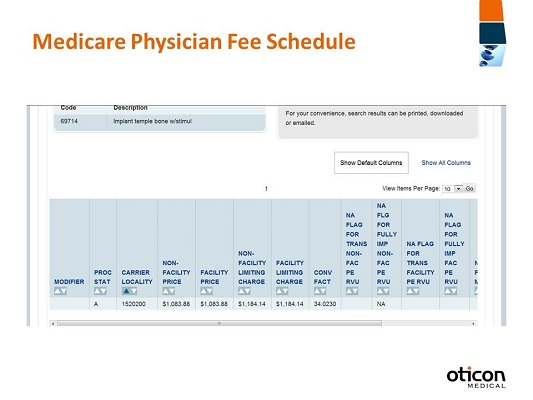
You’ll see in Figure 8 a summary of what we’ve selected for 69714. We can verify that it is the right description. As we page down, we see the different pricing information. What we want to focus on is the facility price, at $1,083.88. That is what the payment rate would actually be in my locality. This is a nice tool to be able to understand your local payment rate.
Figure 8. Search results for Physician Fee Schedule after selecting a procedure and locality.
One of the things that I included today is a link to look up your carrier locality (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ProspMedicareFeeSvcPmtGen/index.html). If you aren’t aware of what your locality might be, Medicare provides a wonderful Excel file that you can get to. This is a link to it so that you are able to look up your zip code and then find which carrier locality would be yours. As we move forward into hospital outpatient reimbursement, or the APCs, when we talk about prospective payment systems, services in each APC are going to be similar, both clinically and in terms of resources they require. Again, Medicare took a look at what resources are required to perform something. The payment rate is going to be established for each APC, so the CPT code that you bill is going to map to the particular APC. That would be the payment rate for the hospital outpatient service; a lot of acronyms I know.
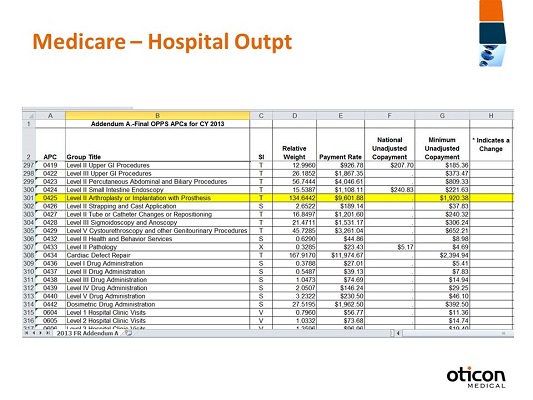
An APC, like I said before, includes everything, inexpensive drugs that are considered packaged, medical/surgical supplies, recovery room, anesthesia and IV therapy. You bill for everything that you are providing, but you’re going to get paid the one lump sum. Significant changes to this reimbursement methodology are published on a yearly basis. Our codes, 69714 through 69718, map to APC 425. Effective in 2013, the national average payment for APC 425 is $9,601.88. Remember, this includes everything, so this is for the surgery and the device for the hospital outpatient. To account for geographic differences, the actual payment is going to be different. It’s going to vary because of the way they calculate the labor portion of their payment. I want to show you how you can look up these payment rates for future reference, and perhaps for other procedures that you perform.
Figure 9 is the page for the perspective payment systems. This is going to be where I spoke earlier about the zip code to carrier locality file. It can be found through this link: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Addendum-A-and-Addendum-B-Updates-Items/January-2013-addendum-A.html It’s an Excel sheet, and you would open it up and be able to page down. You look at your state, find your zip code and then you’re able to find out the carrier code and the locality. It’s nice to know where these resources are on the Medicare page, because there’s so much information.
Figure 9. Medicare hospital outpatient fee schedule addendum.
They released this in January 2013 (Figure 9); it’s the Addendum A for 2013, and if we click on that link then we have to agree to the reverse liability, again. You see the APC column on the left. We want to go down to 425, and then you’ll see the payment rate. So this is a good way for you to look up any other procedures that you might want to inquire about.
We are going to move forward into the ambulatory surgery centers. Medicare also pays for certain procedures in an ambulatory surgery center setting. In the past, there was quite a limited list of items that they would pay for in that setting. However, in the past few years they’ve opened that up to more procedures. An ASC, according to Medicare, is going to be a distinct entity that’s established exclusively for outpatient surgical services so providers that are ASC’s must be certified Medicare providers and as I noted before there is an expanded list of services that can be done. Medicare takes seriously that services can be done based on their safety risks and what medical monitoring is required.
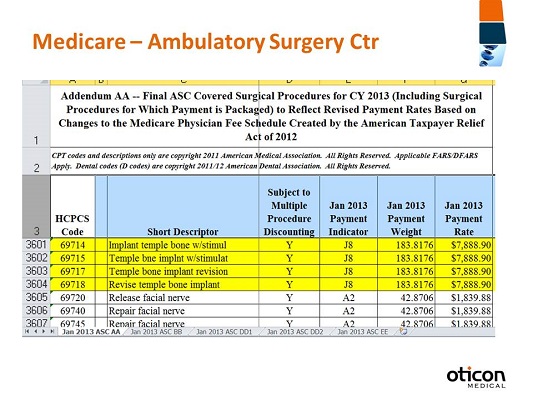
Payment for an ASC is going to be based on the CPT code. The payment amount is going to be less than you would see in an outpatient hospital site of service. Again, these are going to be geographically adjusted, so you’ll see that there will be variation depending on location. In 2013, 69714 through 69718 are going to be reimbursed at $7,888.90 in an ASC. That is encompassing the surgery and the device, so it is less than at the hospital outpatient. Again, remember what we talked about. Medicare is trying to be a savvy purchaser of healthcare - they look at things like what are the costs and what is the overhead in each place of service. So they’ve determined that that would be less at this site of service. Just yesterday I read an article showing that there are some organizations that are trying to advise Medicare that they should level the playing field and make the payments at both sites of service equal moving forward, but we’ll see what happens with those proposed changes.
These reimbursement rates can be found again on the Web site (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/11_Addenda_Updates.html). It’s called Addendum AA this time (Figure 10). Here we have addendum updates for ASC. As you page down, you’ll see that there’s the January 2013 improved list. Like I said before, there have been changes, and there probably will continue to be changes as to what procedures are allowed to be done in an ASC. So they list out those codes as well as the payment rates on this schedule.
Figure 10. ASC covered surgical procedures for 2013.
We verify that this is for 2013, including surgical procedures for which payment is packaged. We will go down and find the CPT code that’s applicable. We are going to be using 69714 for today’s purposes. You’ll see that it is payable at $7,888.90 (Figure 10). I think this is a great resource to be able to know how to get to and to understand what your payment rates are going to be. What’s also important to know is that locality will determine some of your payment rates. I wanted to include information on how to find your local contacts, because I think it’s important to know to go to the Web site of your local MAC and to see what fee schedules are published. Often times they will also publish a local fee schedule for physician reimbursement as well as the ASCs.
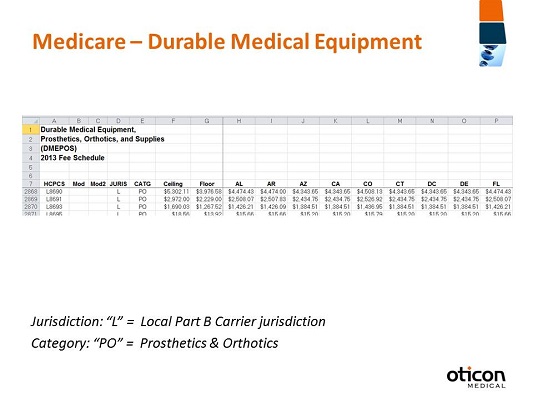
We’re going to move forward into Medicare DME reimbursement. Medicare is going to publish rates and include what’s called a floor and a ceiling rate and also individual state rates that are the reimbursement rates for Durable Medical Equipment, Prosthetics/Orthotics, and Supplies (DMEPOS). For L8691, the floor is $2,229 and the ceiling is $2972. As we all remember, L8692 is not covered by Medicare; that’s going to be the softband with a sound processor, which is considered a hearing aid for Medicare. Then we have the rates for L8693 which are $1,267.52 to $1,690.03. The link for this fee schedule is https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/DMEPOSFeeSched/DMEPOS-Fee-Schedule.html The fee schedule for the ceiling and the floor rates is again going to be found in an Excel worksheet, again (Figure 11). You page through by state to find the applicable reimbursement for the HCPCS code. What can be confusing a bit is that the HCPCS codes for the bone anchored hearing devices are on the DMEPOS fee schedule; yet they are not billed to the local DME. They are billed to the Part B carrier, so you’ll see that noted under jurisdiction on the fee schedule L, Local Part B Carrier Jurisdiction, so that’s where it should be sent. This is the provider compliance map link so that you can access your specific CMS contract information (https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/provider-compliance-interactive-map/index.html).
Figure 11. Durable Medical Equipment fee schedule for 2013.
What’s Next?
We’ve gone through coding, coverage, and payment. They are the cornerstones of reimbursement. They form the foundation to what makes up the whole of reimbursement. From my perspective, from the medical device companies’ perspective, reimbursement is very important. It’s as important as FDA approval or clearance of a device, but as we quickly reviewed, you simply can’t have a device cleared or approved by the FDA and expect to see it used in the marketplace. You need to have that coding and coverage, and the payment needs to be established and be one that is acceptable. Even just having coding doesn’t guarantee anything. You need to also have both coverage and payment. That’s why it’s really important to understand all three of these concepts.
The coverage policies are going to have a major impact on whether or not healthcare marketplace adopts technologies or services, and as we noted quite often today, Medicare is looked to as the precedent for these decisions. Even though there isn’t an obligation for other payers to follow what Medicare says, many do. They look at them as a precedent for when they make coverage decisions, as well as how they make payments, what payment rates are, and what methodologies they use. Hopefully this was a good review of that process. Obviously, we could have gone into it in more detail.
What I wanted to do quickly is talk about how these all factor into the real world. We’ve watched the presentation, we’ve seen our patients, and we’ve identified some patients that we think are candidates for bone-anchored hearing devices. So what is next? What do we do? What’s important is to understand who the payer is going to be for the candidate and to contact them. You always want to make sure that the information you have is accurate, that the patient is still going to be covered, that they’re a covered member of that payer, and then you talk to the payer and understand the benefit information and the coverage information. We know the specific codes that would be used to identify the diagnosis of the patient, as well as what procedure we want to do, what devices we want to use. What we always want to make sure, too, is that are we an in-network provider or an out-of-network provider, because benefits can vary based on that.
You find out what is needed in order for coverage to occur and provide any required medical necessity documentation. I think what’s also important, especially if you haven’t seen many patients or had many bone anchored procedures is to understand your payment methodologies. If your contracts were established quite some time ago for private payers, you may want to revisit them and see how the reimbursements are calculated and see what the reimbursement amounts might be in place. I think it’s also important to remember that you need to find out if there’s a procedure in place for preauthorization or precertification. Are those required? Is it necessary for you to have the procedure authorized? Sometimes outpatient procedures don’t require an authorization, but you still might want to push to make sure that there is going to be coverage in place for this for the procedure and the device.
One thing I want to always remind everyone to do is document, document, document. Always document the contact person that you’ve spoken with, the date and time, summarize your conversation, and any reference numbers to specific calls. I know when I speak with folks at different Medicaid plans, I get a reference number for each of my calls that take place. You want to know that there might be a reference number for any call you make. Also, if you do go through a preauthorization process or have to get a precertification, you want to document that that has been established in case you have any issues moving forward.
Summary
This might seem like a lot. It’s bringing together the whole concept of understanding the coding, the coverage and what you’re going to get paid. That’s why Oticon Medical wants to remind you that we do assist our customers with insurance support. We have a department that will help assist in the process of determining coverage and also obtaining any necessary preauthorizations. If you contact us at Oticon Medical (1-888-277-8014) we will talk to you about the process. We will provide you with some forms that you would need to complete on your practice as well as on the patient, and then, of course, some privacy waivers would be necessary. We look to you to provide the medical necessity information because you’re the provider. It’s important that, as the healthcare provider, you document why the candidate would be a candidate for the treatment. Then, on behalf of you, as well as the patient, we try to determine if coverage is available. We would contact the payers and do our best to get any authorization that might be needed in order for the procedure to take place or even for the softbands and the sound processors to be authorized, not necessarily just the surgery. Please feel free to contact our insurance support specialists. It might take away some of the frustration that you find.
It’s very exciting to know that Oticon Medical is now a Medicare Durable Medical Equipment provider. We have become a provider just recently. We think it’s very important to become one because many patients, as I noted earlier, are at a point where they find that they need a replacement sound processor. Because the laws that are in place don’t allow many physicians to provide DME out of their office, with very few exceptions, it’s important that we become credentialed as a Medicare DME provider. Patients would therefore contact Oticon Medical. We would walk them through the process of what they need to do. Right now we can bill for traditional Medicare, and we are working on establishing provider agreements with the various state Medicaid plans as well.
We think it’s important that if a patient comes into your office and they find that it’s time for a replacement sound processor that they try on the equipment that’s out there. We want to make sure that we are there to help them to get what they need and what they want. Please remember that you can contact us for that reason as well. Our territory managers and our clinical managers can also walk you through the process of what we can do to help.
Please feel free to reach out to me at the phone number or the e-mail listed in your handout. I am happy to talk to you about your reimbursement concerns or questions with regard to bone-anchored hearing systems. As I mentioned earlier, we want to be a resource for you, so when you run into some obstacles, please know that you can contact either me or our reimbursement specialists in our office. Thank you, and I appreciate your time.
Cite this content as:
Hart, C. (2013, May). Reimbursement and bone anchored systems. AudiologyOnline, Article #11830. Retrieved from https://www.audiologyonline.com/